Point your compass toward your dream
Adventure Awaits. Discovery Awaits. Your future awaits at Ohio Northern University –
the place to find True North!

#1 in Ohio, #2 in the Midwest
New Wall Street Journal and U.S. News & World Report rankings list Ohio Northern University as a top college for providing an exceptional and affordable education. ONU is ranked No. 2 in U.S. News & World Report’s Best Regional Colleges Midwest list for 2024, making it No. 1 in Ohio, and places highly in other key categories, including 3rd (first in Ohio) in regional Best Value Schools. The WSJ/College Pulse 2024 Best Colleges in the U.S. ranks ONU No. 33 in the nation and No. 1 in Ohio for “salary impact.”
By the numbers
There are lots of things we want you to know about Ohio Northern, but here are a few to get you started.
-
12:1 Student-faculty ratio
-
19 Average class size
-
50,000 Yearly volunteer and service hours by our students
-
$27,800 Average financial aid award
News
Apr.
25
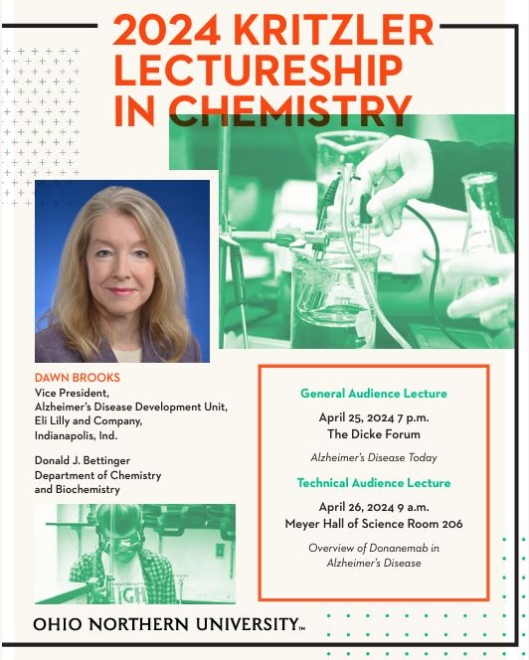
Kritzler Lecture "Alzheimer's Disease Today"
Public Lecture by Dawn Brooks, Vice President, Alzheimer's Disease Development Unit, Eli Lilly and…
Read More- Apr.24
Embracing Neurodiversity in the Classroom
This workshop and discussion will be facilitated…
Read More